A tiny brain-stimulating implant has been demonstrated in people for the first time. More research is needed, but if it works as hoped, it could be a more convenient, less risky way to use neurostimulation to treat people with depression and other neuropsychiatric disorders.
The challenge: About 280 million people worldwide are living with depression, and an estimated 30% of them have treatment-resistant depression (TRD), meaning they don’t feel any symptom relief even after trying two or more antidepressants.
Neurostimulation — the use of electrical implants or external machines to mildly stimulate the brain — has been shown to relieve depression symptoms for some people with TRD.
“We’ve developed what we believe is the smallest implantable brain stimulator demonstrated in a human subject.”
Jacob Robinson
However, getting a brain implant is a serious procedure — typically, doctors will open up a patient’s skull to insert the device, and then run wires under their skin to a battery in their chest.
Because external neurostimulation devices need to be powerful enough to work from outside the skull, they’re only approved for use in clinics, and a person may need to commit to clinic appointments as often as five days a week for up to six weeks.
What’s new? Houston-based startup Motif Neurotech is developing a pea-sized brain implant that takes just 20 minutes to insert, in an out-patient procedure. It can easily deliver neurostimulation in a person’s home, eliminating the need for regular clinic visits.
The startup recently shared a paper detailing the first two in-human demonstrations of the device, as well as data from pig tests lasting up to 35 days, on the preprint server medRXiv.
“We’ve developed what we believe is the smallest implantable brain stimulator demonstrated in a human subject,” said Jacob Robinson, Motif’s CEO and founder. “Our wireless, battery-free device will enable a minimally-invasive neurostimulation solution to treat neuropsychiatric diseases such as TRD.”
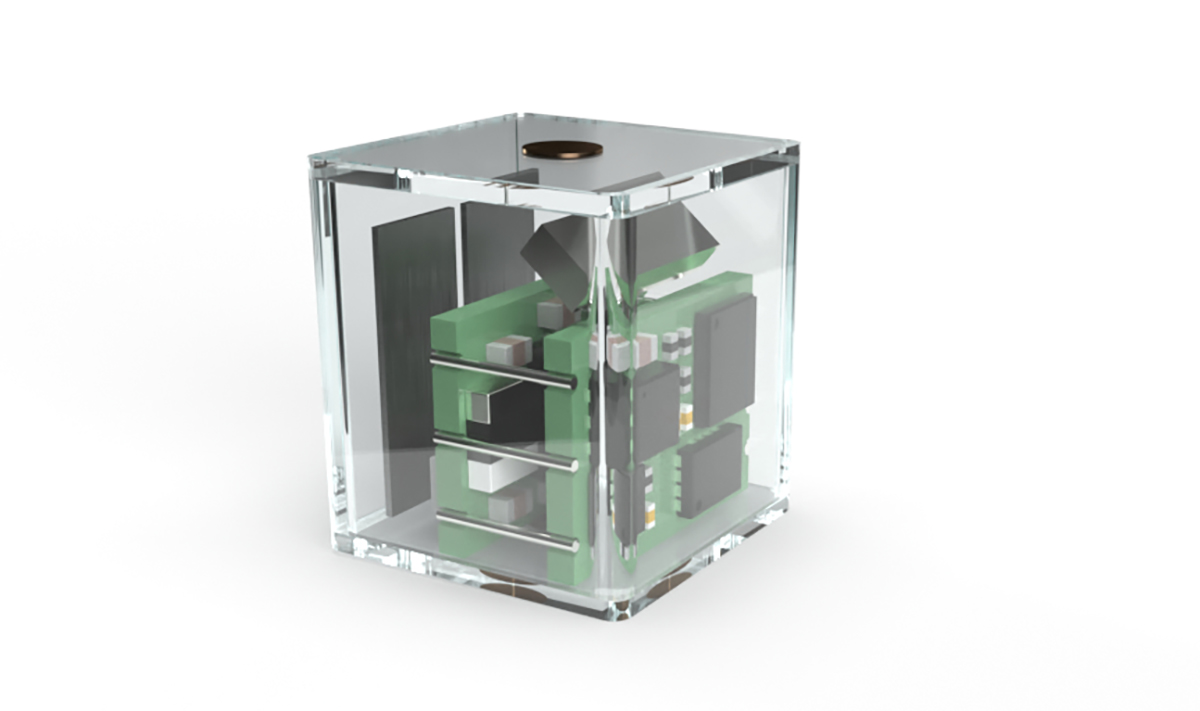
How it works: To implant the device, surgeons pull back the skin over part of a person’s skull and drill a small hole in the bone without going all the way through it or exposing the brain. They then place the implant into the skull itself, add a cover, and reattach the skin.
To treat TDS, a person would put on a headset that can emit a magnetic field. This causes a magnetoelectric material in the brain implant to vibrate, and another part of the implant turns those vibrations into electricity.
First steps: During the in-human tests — which involved two patients already having brain tumor removal surgery — the implant was placed over a part of the brain that controls movement for just a few minutes.
A wand was then used to deliver the magnetic field needed to trigger the brain implant. This caused the muscles in the patients’ hands to twitch.
When the implant was tested in pigs, the researchers also targeted a part of the brain controlling movement, though in those studies, the device was left in the animals’ skulls for up to 35 days.
In both cases, the tests show that the device is capable of neurostimulation, but they don’t tell us if it can treat TRD as effectively as other methods — or at all.
“We see a path to treat psychiatric and neurological disorders with short out-patient procedures.”
Woods et al. (2023)
Looking ahead: Motif is still developing the headset needed to enable at-home neurostimulation, but is hopeful its system will be ready for feasibility studies in 2025.
If it works as hoped for TRD, it could potentially be used to treat other disorders known to respond to brain stimulation, too, such as Parkinson’s, Tourette’s, and OCD.
“With these tiny battery-free neuromodulation devices, we see a path to treat psychiatric and neurological disorders with short out-patient procedures that result in simple, long-lasting, therapies with very few side effects when compared to drugs,” write the Motif researchers.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].





