Researchers at Tampa’s Moffitt Cancer Center have used a herpes virus to fight triple-negative breast cancer — and the results from a new phase 2 clinical trial are promising.
Combined with standard chemotherapy and given before surgery, the team found that the modified virus, called TVEC, led to an increase in signs of an immune system response to the tumor, and it seemed tied to an improved rate of survival compared to chemo on its own.
The therapy also showed no signs of the autoimmune toxicity that immunotherapy patients may experience.
“Our results demonstrate that TVEC, when added to systemic chemotherapy, may increase responses in high risk, early stage triple-negative breast cancer,” Hatem Soliman, lead author of the study, medical director of the Clinical Trials Office at Moffitt and senior member of the Breast Oncology Department, said in a statement.
“There is evidence of robust immune activation within the tumor, and additional investigation of TVEC in combination with current chemoimmunotherapy for triple-negative breast cancer is warranted.”
Researchers have announced promising results of a phase 2 trial testing a cancer-killing herpes virus, TVEC, against triple-negative breast cancer.
What is triple-negative breast cancer? Accounting for around 15% of newly diagnosed cases, triple-negative breast cancer is described in the study, published in Nature Medicine, as particularly dangerous and a “major therapeutic challenge.”
Tumor cells from triple-negative breast cancer don’t express any of three important receptors — estrogen, progesterone, or a protein called HER2 — which are commonly found on other breast cancers and help regulate their growth.
Many drugs target these receptors to stop the cancer from growing, but they don’t work very well with triple-negative breast cancer. Instead, clinicians must rely more on blunter tools like radiation and cytotoxic chemotherapy. More recently, this regimen has begun to be combined with Keytruda to ramp up the immune system.
While it can work, this mainline defense has serious side effects.
“This is just a terrible disease, and outcomes until the last five years have just been so terrible,” Yuman Fong, a cancer immunotherapy researcher and chair of the surgery department at the City of Hope cancer center, told STAT’s Angus Chen.
Viruses to the rescue: Cancer patients now have options beyond radiation, chemotherapy, and hormone therapy — most notably immunotherapy, which leverages the body’s own immune system to fight cancer.
Researchers have also begun drafting a new ally: viruses.
Triple-negative breast cancer is considered especially difficult to treat, as it lacks three targets cancer therapies take aim at.
Certain viruses, known as oncolytic viruses, have a proclivity for infecting and killing cancer cells, and numerous studies have shown promising results by turning the little nasties loose on cancer and letting them do what they do best.
Studies have looked at using viruses and immune system cells together (kind of like Spider-Man and Doctor Octopus teaming up to take on a bigger threat), using Ebola to battle tumors in the brain, and harnessing herpes simplex 1 (HSV-1) to fight childhood brain cancer and other rare cancers.
Cancer killer: The TVEC virus used in Moffit’s phase 2 trial is an engineered version of HSV-1, and it’s a double-barrelled cancer killer. (The virus therapy has previously won approval to treat advanced late stage melanoma.)
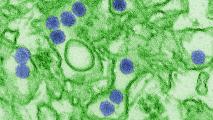
First, TVEC directly attacks and kills malignant cells. Viruses can be especially deadly to cancer cells because the cells have turned off some of the antiviral defenses that healthy cells have, Soliman told STAT.
Second, when the tumor cells are exploded by viruses, they release yet more targets the immune system can recognize, helping to call in further reinforcements from immune cells.
But TVEC isn’t done when the tumor cell is. The virus is also engineered to produce a protein called GM-CSF, which serves as another signal flare for the immune system to come find its targets.
“The patrolling cells gobble up the tumor-associated antigens and allow the immune system to say, ‘Hey, this is something we need to engage,’” Soliman told Chen. “That’s one idea behind oncolytic viruses — reawaken the immune system to tumor-associated antigens that it may have been ignoring previously.”
“Our results demonstrate that TVEC, when added to systemic chemotherapy, may increase responses in high risk, early stage triple-negative breast cancer.”
Hatem Solimon
The study: The phase 2 trial was designed to see if TVEC could be effective in triple-negative breast cancer patients when combined with normal chemotherapy pre-surgery.
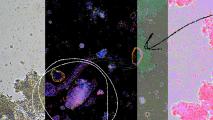
The 37 patients received 12 weeks of chemotherapy before surgery, as well as multiple injections of the virus directly into their tumors, Chen explained. The team took biopsy samples before treatment, at the halfway point, and then again post-surgery.
The biopsies revealed the presence of immune cells in the tumors, a signal that TVEC was working, and 45.9% of patients showed a response to the therapy, meaning their tumors were dead by the time they had surgery, Fong told Chen. Two years after the treatment, 89% of patients had no recurrence, compared to the typical 60% rate for patients on chemotherapy alone and the typical 84% rate for chemo plus Keytruda, taken over three years.
Importantly, this study was small and lacked a control group, so the comparison to the recurrence rates for the population at large may not be represenative. But Soliman hopes to begin a larger, randomized trial next, which will test if adding TVEC to chemo and a Keytruda-like drug can boost the efficacy even higher.
If adding the cancer-killing virus works, the hope is that this will allow clinicians to use less chemo, while allowing the immune system to do more of the work.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].