Researchers have essentially cured type 1 diabetes in monkeys, using bioengineering and a new transplant technique. They hope it will fundamentally change the way the chronic disease is treated.
Led by researchers from Massachusetts General Hospital’s Center for Transplantation Science, the experiment cured the disease, an autoimmune condition in which the body cannot produce insulin, in three non-human primates — at least, for the duration of the 90-day study.
“The application of this strategy, particularly in stem cell-based therapy, has the potential to revolutionize the paradigm for treating patients with type 1 diabetes,” said transplant surgery chief James F. Markmann.
Researchers have bioengineered a new transplant technique they hope will fundamentally change the way type 1 diabetes is treated.
Transplants and diabetes: The American Diabetes Association estimates that 1.9 million people in the US have type 1 diabetes, including around a quarter million adolescents. In type 1 diabetes, people do not have the ability to make insulin — the pancreatic cells that create insulin are missing; the leading theory is that the immune system goes rogue and destroys them.
With little to no insulin being produced, people with type 1 diabetes require lifelong injections of artificial insulin to avoid dangerous blood sugar levels. Before the invention of insulin shots, the disease was fatal.
There are treatments that could potentially eliminate the need for shots, though, by transplanting tissues could restore the ability to make insulin again.
With little to no insulin being produced, people with type 1 diabetes require lifelong injections of artificial insulin. There are treatments that could potentially eliminate the need for shots, though, by transplanting tissues could restore the ability to make insulin again.
There are two potential transplants for diabetes patients: in one, the entire pancreas of a donor is transplanted. This is currently approved by the FDA, but total organ transplant is a major surgery, and the risks are significant. As a result, pancreas transplants are rare — with only about 1,000 performed each year — and reserved for patients with the most severe conditions, which can’t be managed with insulin.
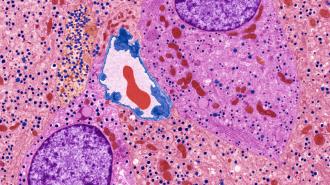
Much less invasive is an islet allotransplant, where surgeons only transplant smaller pancreatic “islets” — groups of cells in the pancreas that are home to the insulin-producing beta cells.
These islets are then typically transplanted into the patient’s liver. It may take multiple tries to get them to stick, but if they do, patients may find they no longer need to inject insulin — or can use less.
But islet transplants are still considered experimental procedures, so they can only be done as part of a clinical trial. As a result, they are even rarer than whole pancreas transplants. From 1999 to 2020, only 1,399 people have received the procedure, according to a global registry of islet transplants, and only a couple dozen attempts are made worldwide each year.
A new site: While islet transplants can work, a variety of issues hold it back.
One issue is the location in the liver: the immune system can still end up destroying as many as half of the transplanted beta cells there, and the liver itself has limited room for transplanted tissue. (It’s also difficult to monitor and hard to remove the islets if something goes wrong.)
Mass General researchers set out to find a better spot for the islets. They settled on a fold of fatty tissue called the omentum, which begins around the stomach and lays across the intestines.
In the monkey experiment, published in Cell Reports Medicine, the team used an enzyme that stops bleeding and the monkey’s own blood plasma to create a kind of “matrix” that allowed the pancreatic islets to stick to the omentum; the matrix then naturally biodegrades.
When they combined their new transplant technique with immunosuppressant therapy, they were able to effectively cure type 1 diabetes in monkeys.
When they combined the transplant with immunosuppressant therapy to protect the new cells, the diabetic monkeys were able to make their own insulin and automatically stabilize their blood sugar levels.
It is “the first time that such a demonstration has been made in a nonhuman primate model,” study first author Hong Ping Deng, a researcher of transplant surgery at Mass General, said.
A better cure: Even with the new technique, islet transplantation still has a number of challenges to overcome. It still requires immunosuppressants, which have a long list of complications and side effects, and it still requires a compatible organ donor — and donor pancreases are in extremely short supply.
However, there’s one more type of transplant that cured the first person in history of type 1 diabetes in 2021: an infusion of islets derived from embryonic stem cells.
While stem cells could provide a theoretically endless supply of islets for transplant, there are concerns about this type of transplant too, including the potential for rejection and the possibility of tumor growth.
But researchers behind this study say that the omentum may make for an attractive site for future stem cell transplants, as well, because it is much easier to monitor than the liver and is non-vital, so transplanted tissue is easier and safer to remove if complications arise.
A clinical trial is now being planned to test the technique in humans.
Editor’s note: Corrected 3/9/2023. This story originally described type 1 diabetes as a condition in which people are born without the ability to make insulin; this isn’t correct. While the condition has a genetic component, symptoms typically develop in childhood but can begin at any age, and environmental factors may also play a role in triggering the condition.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at tips@freethink.com.