Moderna’s new mRNA cancer vaccine significantly reduced skin cancer patients’ risk of recurrence or death compared to a standard treatment alone, according to the newly announced topline results of a phase 2 trial.
“mRNA has been transformative for COVID-19, and now, for the first time ever, we have demonstrated the potential for mRNA to have an impact on outcomes in a randomized clinical trial in melanoma,” said Moderna CEO Stéphane Bancel.
The background: In October 2022, pharma giant Merck gave Moderna $250 million to co-develop and commercialize mRNA-4157, a personalized mRNA cancer vaccine it first began investing in back in 2016.
The new investment came while mRNA-4157 was still in the later-stages of a phase 2 clinical trial involving 157 people with high-risk melanoma who’d had their tumors removed via surgery.
Every year, nearly 100,000 people in the US are diagnosed with melanoma.
During the trial, participants received 9 doses of the vaccine (administered every 21 days) and 18 doses of Merck’s FDA-approved cancer treatment, Keytruda (also administered every 21 days), or just the Keytruda.
They were then monitored for at least two years or until their cancer came back. The purpose of the trial was to test the efficacy of the mRNA cancer vaccine at preventing recurrence or death when administered alongside Keytruda compared to Keytruda alone.
What’s new? Moderna and Merck have now announced that the addition of mRNA-4157 reduced trial participants’ risk of recurrence or death by 44%, compared to standard treatment, meeting the goal of a statistically significant and clinically meaningful reduction.
The trial was relatively small, but the companies say they plan to work with regulators to launch a larger phase 3 trial of melanoma patients in 2023.
The phase 2 results still have to undergo peer review, too, but Moderna and Merck say they plan to submit them to a medical journal for publication. They also plan to share more specific trial data at an upcoming oncology meeting.
“We’re not adding undue processes that would negatively impact the patient.”
Michelle Brown
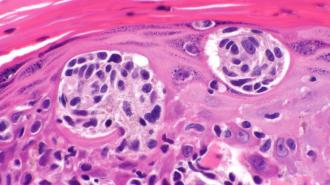
How it works: Cancer cells have proteins called “neoantigens” on their surfaces. These proteins aren’t found on any other type of cell, and they’re unique to each tumor.
Moderna’s personalized cancer vaccine instructs a patient’s cells to make up to 34 of the neoantigens found on their tumor cells. The immune system can then learn to identify and target these cancer cells, since they are covered in the proteins.
The process of creating the personalized mRNA cancer vaccine starts with a doctor taking a sample of a patient’s tumor and sending it to Moderna. Using digital algorithms, Moderna analyzes the sample to identify the best neoantigens to target before manufacturing the personalized mRNA vaccine.
Moderna then sends the vaccine back to the clinic treating the patient, where it’s administered with an intramuscular injection, like the mRNA vaccines for COVID-19.
“I think one of the things that’s really neat from a scientific perspective is we are making this individual medicine for a specific patient and we’re also not adding undue processes that would negatively impact the patient,” Michelle Brown, Moderna’s program director for oncology, told Freethink.
The whole production process takes just a couple of weeks, according to Brown.
“It is a personalized process — it’s not going to be a couple of days,” she told Freethink. “But if we think about just normal testing for tumors, that can take up to ten days to two weeks.”
“We have had…a lot of years to work through what the manufacturing capability needed to be.”
Kyle Holen
Scaling up: Every year, nearly 100,000 people in the US are diagnosed with melanoma. That’s not a huge number compared to the billions of COVID-19 shots Moderna can produce, but those doses are mostly identical, while the cancer vaccines will need to be designed and produced for one patient at a time.
But Kyle Holen, Moderna’s head of development for oncology, is confident in the company’s ability to scale up production, if mRNA-4157 — and future mRNA cancer vaccines — make it through the development and approval processes.
“We have had…a lot of years to work through what the manufacturing capability needed to be to scale for something like a personalized cancer vaccine,” he told Freethink.
“We believe we can scale effectively to solve, certainly, the melanoma population,” he added. “If we decided to explore other tumor types, like lung cancer or colorectal cancer or triple negative breast cancer, we believe we can scale across all of these indications.”
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at tips@freethink.com.