With so much attention focused on the explosion of progress in artificial intelligence, you’d be forgiven for missing just how incredible the progress has been in medical science, too. Since January, we’ve been rolling out blood screening for cancer and testing gene editing for Alzheimer’s. We’ve developed several new, highly effective drugs for weight loss. But one of the most incredible recent advances has to be around the malaria vaccine.
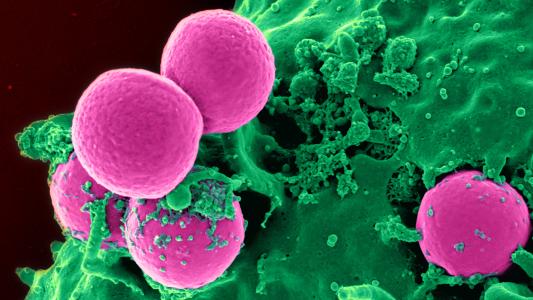
Every year, around 250 million people get malaria, with around 620,000 people dying from it — the vast majority of them children. Ninety percent of all malaria deaths occur in sub-Saharan Africa, and malaria often imposes long-term health complications. In countries like Kenya, Nigeria, and Ghana, malaria devastates economies and burdens communities. A child will die from malaria every two minutes.
So, when we got the news of a highly effective and easily produced malaria vaccine, called R21, it was cause for celebration. This new vaccine, developed by Oxford University, was found to be much more effective than the previous best vaccine, made by GSK. As Freethink reported, “In early trials, the vaccine looked to be 77% effective against severe cases of malaria up to a year after dosing — compared to just 30% for the GSK vaccine endorsed by the [World Health Organization (WHO].”
The WHO, however, says the vaccines haven’t been compared head-to-head and expects them to have similarly high efficacy when given right before malaria season. Either way, R21 is universally acknowledged to be much cheaper than GSK’s shot, and it will radically increase the supply of malaria vaccines.
“Why would you allow children to die?”
Recently, though, this scientific and medical success story has hit a bureaucratic wall. The WHO is coordinating the rollout of this new R21 malaria vaccine. Oxford University says it has provided the WHO with all the data they need to evaluate it. Ghana and Nigeria’s health authorities have approved the shot. By all accounts, the Serum Institute of India – the world’s largest manufacturer of vaccines – is ready to go.
The Serum Institute has manufactured 20 million doses of R21 so far and “has already established production capacity for 100 million doses per annum, which will be doubled over the next two years.” The WHO endorsed the vaccine earlier this month and said the shot has been shown to be safe, highly effective, high-impact, and cost-effective.
It came as quite a shock, then, that the WHO has decided to wait several months to distribute the jab and is only targeting distribution by mid-2024. Adrian Hill, the Director of the Jenner Institute at Oxford University, is incredulous.
Hill told the Financial Times, “Why would you allow children to die instead of distributing the vaccine? There’s no sensible answer to that — of course, you wouldn’t. … There’s plenty of vaccine, let’s get it out there this year. We’ve done our best to answer huge amounts of questions, none of which a mother with a child at risk of malaria would be interested in.”
The WHO told the Financial Times that mid-2024 is a “conservative” estimate and hopes that it will be rolled out sooner. But every month’s delay means potentially thousands of children may die from malaria unnecessarily.
Isn’t this an “emergency”?
The WHO’s slow movement on malaria is all the more perplexing when you compare it with how quickly the COVID-19 vaccines were reviewed, approved, and distributed. The need is urgent: close to half a million children under the age of five will die from malaria this year.
Oxford’s Hill makes the comparison explicit. While COVID-19 vaccines were distributed “within weeks” of approval, he says, tens of millions of doses of R21 are just sitting in a fridge in India. Hill told the Financial Times, “We’d like to see the same importance given to the malaria vaccine [as COVID] for children in Africa. … We don’t think this would be fair to rural African countries if they were not provided with the same rapidity of review and supply.”
The WHO says it agrees “everything should be done” to expedite the process, which it says is essential for “safety, quality and trust,” but it isn’t clear why things aren’t in fact moving as fast as they did for COVID-19 or what needs to happen to go faster.
Two biases may be at play here.
The first is a damaging and depressing application of “novelty bias,” where we place more emphasis on new experiences or dangers than old and familiar ones. We’ve always had malaria. we’ve always had malaria deaths. COVID-19 was new, so it was treated with special attention and urgency. We’re wired to not see something as an “emergency” if it happens every year — even if hundreds of thousands are dying from it. The novel coronavirus emerged in late 2019, and the first vaccines were approved in late 2020. Malaria vaccine research has been going on for decades, so a delay of several months doesn’t seem like much.
The second potential bias is the fact that while malaria deaths are overwhelmingly concentrated in sub-Saharan Africa, COVID-19 affected far more people around the world. It also affected richer and more developed countries, where vaccine rollout would be more lucrative for pharmaceutical companies.
There seems to be little reason to delay the distribution of the malaria vaccine, especially given that we’ve now seen how rapidly it could be done, when the world puts its collective mind to it.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].