MIT engineers have developed a telerobotic system to help surgeons quickly and remotely treat patients experiencing a stroke or aneurysm. With a modified joystick, surgeons in one hospital may control a robotic arm at another location to safely operate on a patient during a critical window of time that could save the patient’s life and preserve their brain function.
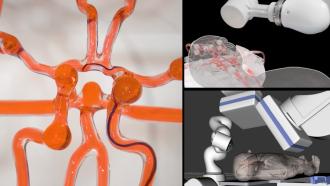
The robotic system, whose movement is controlled through magnets, is designed to remotely assist in endovascular intervention — a procedure performed in emergency situations to treat strokes caused by a blood clot. Such interventions normally require a surgeon to manually guide a thin wire to the clot, where it can physically clear the blockage or deliver drugs to break it up.
One limitation of such procedures is accessibility: Neurovascular surgeons are often based at major medical institutions that are difficult to reach for patients in remote areas, particularly during the “golden hour” — the critical period after a stroke’s onset, during which treatment should be administered to minimize any damage to the brain.
The MIT team envisions that its robotic system could be installed at smaller hospitals and remotely guided by trained surgeons at larger medical centers. The system includes a medical-grade robotic arm with a magnet attached to its wrist. With a joystick and live imaging, an operator can adjust the magnet’s orientation and manipulate the arm to guide a soft and thin magnetic wire through arteries and vessels.
The researchers demonstrated the system in a “phantom,” a transparent model with vessels replicating complex arteries of the brain. With just an hour of training, neurosurgeons were able to remotely control the robot’s arm to guide a wire through a maze of vessels to reach target locations in the model.
“We imagine, instead of transporting a patient from a rural area to a large city, they could go to a local hospital where nurses could set up this system. A neurosurgeon at a major medical center could watch live imaging of the patient and use the robot to operate in that golden hour. That’s our future dream,” says Xuanhe Zhao, a professor of mechanical engineering and of civil and environmental engineering at MIT.
Zhao and his team have published their findings today in Science Robotics. MIT co-authors include lead author Yoonho Kim, Emily Genevriere, and Jaehun Choe, along with Pablo Harker, Robert Regenhardt, Justin Vranic, Adam Dmytriw, and Aman Patel at Massachusetts General Hospital (MGH), and Marcin Balicki of Philips Research North America.
Tilt and twist
Endovascular surgery is a specialized, minimally invasive procedure that involves carefully twisting and guiding a thin medical wire through the body’s arteries and vessels to a target location, in a way that avoids damaging vessel walls. The procedure typically requires years of training for a surgeon to master.
Robotic systems are being explored as assistive technologies in endovascular surgery. These systems mainly involve motor drives that advance and retract a wire while twisting it through the body’s vasculature.
“But having a robot twist with the same level of sophistication [as a surgeon] is challenging,” Kim notes. “Our system is based on a fundamentally different mechanism.”
The team’s new system builds on work from 2019, in which they demonstrated steering a magnetically controlled thread through a life-sized silicone model of the brain’s blood vessels. They did so at the time using a handheld magnet, about the size of a soup can, that they manually manipulated.
They have since affixed the magnet to the end of a medical-grade robotic arm, which can be steered using a small joystick knob on a mouse. By tilting the joystick, researchers can tilt the magnet in an orientation that a magnetic wire can follow. Buttons on the mouse control a set of motorized linear drives, which advance and retract the wire to make it move forward and back.
The wire is as thin and flexible as a conventional neurovascular guidewire, with a soft, magnetically responsive tip that follows and bends in the direction of a magnetic field.
Finding a path
The team tested the robotic system in MGH’s Catheter Lab — an operating room with standard medical imaging equipment used in endovascular procedures. The researchers installed the robotic arm in the lab, along with a life-sized silicone model of blood vessels. They set the joystick, along with a monitor displaying a live video of the model, in a control room. From there, an operator watched the video while using the joystick to remotely steer the wire through the vessels.
The team trained a group of neurosurgeons to use the robotic system. After just one hour of training, each surgeon was able to successfully operate the system to guide the wire through complex vessels that are difficult to navigate with a manual guidewire.
The team also used the robotic system to clear simulated clots in difficult-to-reach areas in the model. They steered the guidewire through vessels, and around sharp corners and turns, to reach regions where the researchers simulated clots. Once they guided the wire to the clot, the surgeons proceeded with standard endovascular methods to thread a microcatheter along the wire to the site of the clot. They retracted the wire, leaving the catheter, which they then applied to successfully remove the clot.
“The primary purpose of the magnetic guidewire is to get to the target location quickly and safely, so that standard devices like microcatheters can be used to deliver therapeutics,” Kim says. “Our system is like a pathfinder.”
He hopes that the teleoperated system can help more patients receive time-critical treatment. He also sees benefits for surgeons, who typically perform such vascular procedures in the same room as the patient, while being exposed to radiation from X-ray imaging.
“The neurosurgeons can operate the robot in another room or even in another city without repeated exposure to X-rays,” Zhao says. “We are truly excited about the potential impact of this technology on global health, given that stroke is one of the leading causes of death and long-term disability.”
This research was supported in part by the National Science Foundation, the National Institutes of Health, and Phillips Research of North America.
Republished with permission of MIT News. Read the original article.