After spending more than 30 years of his life fighting the AIDS crisis, Wayne Koff found himself coming to a startling realization: namely, that we understand far more about how the HIV virus evolves and adapts over time than we do about how our own immune system responds to it.
“I spent a long time on HIV vaccine development,” says Koff, adjunct professor of epidemiology at the Harvard T.H. Chan School of Public Health. “None of them worked, and slowly, over time, we began to see that we understood a lot about HIV at the molecular level, but we didn’t know anything about ourselves. And the reason is that the immune system is incredibly complex.”
“Progress has been slow because of our lack of understanding of how the immune system works.”
Wayne Koff
This prompted Koff to launch the Human Immunome Project, a groundbreaking plan to use artificial intelligence to create a virtual simulation of the human immune system — in all its complexity — over the next decade. If it succeeds, the potential impacts could be enormous, from improving the effectiveness of cancer therapies to shedding new light on the ongoing mystery of Long Covid.
“We have a range of diseases where, at the core, progress has been slow because of our lack of understanding of how the immune system works across people of different ages, genders, and ethnicities, as well as diversity in terms of genetics and environmental exposures,” says Koff.
The most complicated atlas ever drawn
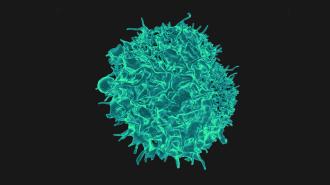
The scale of this challenge is exponentially greater than the Human Genome Project, the international effort to sequence all 3 billion base pairs in human DNA and map all 20,000 human genes, which took more than a decade to complete. The data in the human immunome is millions of times larger and vastly more complex. It does not merely include the legions of lymphocytes, neutrophils, and monocytes/macrophages, which biologists have pieced together and studied over many decades, but all of the interactions these cells have, over a person’s life, with pathogens, toxins, and the consequences of their diet and lifestyle.
How all of this shapes an individual’s immunity does not just vary from person to person based on their genetics and exposures but is constantly shifting over the course of their lifetime.
“The immune system is constantly adapting based on our exposures and experiences,” says John Tsang, an immunobiology professor at Yale School of Medicine. “This makes it so much more complicated than the human genome.”
The data in the human immunome is millions of times larger and vastly more complex than the human genome.
At a population level, Koff describes everyone’s immune system as lying somewhere on a bell-shaped curve. On this curve, one extreme represents immunosuppression — such that the person is very vulnerable to infections and cancer — while the other extreme is excessively immunoreactive, resulting in autoimmune diseases such as multiple sclerosis or type 1 diabetes.
One arm of the Human Immunome Project, known as the Human Immunomics Initiative, is attempting to understand how our place on this bell-shaped curve varies with age, making older people more vulnerable to respiratory infections and the reactivation of dormant pathogens.
To study this, Koff and his collaborators around the world are using existing samples, stored in biobanks, and sequencing vast numbers of crucial lymphocytes, known as B and T cells, each of which contains a unique receptor to recognise parts of viruses, bacteria, or tell-tale signs of cancer cells. Koff’s aim is to create an atlas of these receptors, and feed that information into an AI model to predict what the complete repertoire of B and T cells might look like in young, otherwise healthy individuals, what changes as we age, and what we might be able to do to modulate it.
“Getting to the point where we have shared data from tens of thousands of individuals around the world … is not trivial.”
Shai Shen-Orr
As we age, our responsiveness to vaccines typically declines, and the initiative is attempting to understand why by training machine-learning algorithms on data collected during major vaccine trials. In 2021, they used a vast array of information, ranging from gene expression measurements to immune cell composition, to train an AI model that was capable of predicting immune responses to the hepatitis B vaccine in a small cohort of middle-aged and older adults in Canada.
But immunity also varies substantially around the globe. Shai Shen-Orr, an immunology professor at the Technion – Israel Institute of Technology, points to the example of rotavirus vaccines that are highly effective in Europe and the US but much less so in South Asia. As yet, no one really understands why.
Collecting the data to understand phenomena such as this will require an unprecedented level of collaboration between research laboratories. “Right now, most of the data we have comes from developed countries, but the immune system is all about variation,” says Shen-Orr. “And getting to the point where we have shared data from tens of thousands of individuals around the world for the cumulative benefit of humanity is not trivial.”
The secret to being born
Such data sharing is already underway in another arm of the Human Immunome Project, called Born Strong, which aims to understand and find new ways of preventing pregnancy complications such as miscarriages and preterm birth.
Tobias Kollmann, a pediatric infectious diseases specialist at the Telethon Kids Institute in Perth, who is leading the Born Strong initiative, describes such outcomes as “the longest, deadliest pandemic that we’re dealing with in human history.” It is also one heavily linked to the vagaries of the immune system.
Because the fetus contains a mixture of the father and the mother’s genetics, scientists still do not fully understand how it is able to implant itself within the mother without being immediately rejected by her body. “If you transplant an organ that is half-foreign, it will be thrown out within a matter of hours,” says Kollmann. “So pregnancy is really this massive miracle which we do not fully understand.”
“You need AI because of the scale of the complexity of all this.”
Tobias Kollmann
The secret to how pregnancy happens and why it sometimes fails is thought to lie in the complex network of immune processes that occur in the thin layer of endothelial cells within the uterus, which separates mother from baby. Animal models have suggested that pregnancy loss can be greatly reduced by stabilizing the endothelial cells, and Born Strong have partnered with five different clinical trials taking place around the world from Kenya to Adelaide to investigate various cheap, low-cost interventions.
One of these trials, called AGREE, is taking place in Kisuma, Kenya, where 3,000 pregnant women are enrolled in a trial to test whether a protein supplement called L-arginine can reduce preterm birth. A similar trial in Australia is testing supplementing pregnant women with Omega-3 fatty acids.
But by collecting data from each of these women — sequencing their B and T cell receptors and feeding a vast range of data, from genomics to protein levels, into an AI — Kollmann and his colleagues are hoping to identify some of the key elements of the immune system that are necessary for a successful pregnancy and gain clues regarding the best ways of stabilizing immunity and preventing complications.
“Our hope is that we could potentially narrow this down to one or two drugs or supplements or vaccines, that would work to take care of the vast majority of pregnancies in the world,” he says. “Something which is cheap and can be given as a prophylaxis. But you need AI because of the scale of the complexity of all this. The computer has to progressively learn from the findings of each trial and keep on going.”
“What is it about the aging immune system which makes older people vulnerable?”
Wayne Koff
Koff hopes that Born Strong can provide a blueprint for the kind of data sharing and collaboration that is needed to make the entire Human Immunome Project a success.
If it succeeds, the findings could be transformative for human health.
“When we look at the Covid-19 pandemic, the vast amount of the morbidity and mortality was in the elderly,” he says. “So what is it about the aging immune system which makes older people vulnerable? What are the defects, and can we identify them and modulate them so that our vaccines and drugs work as well in over-80s as they do in younger adults?”
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at tips@freethink.com.