An ear sensor successfully alerted doctors to signs that COVID-19 patients isolating at home should be hospitalized — even when the patients themselves didn’t realize their conditions had gotten that bad.
Monitoring COVID-19 patients: A mild case of COVID-19 can turn into a life-threatening one within days, so it’s important for doctors to monitor patients for signs their condition is worsening — the sooner they spot these signs, the sooner they can administer more aggressive treatments.
It’s not possible to monitor every high-risk COVID-19 patient in-person at a hospital, though — the facilities are already too easily overwhelmed, plus each additional COVID-19 patient in a hospital increases the risk of spreading it to other patients and staff.
A patient might not feel worse until after their illness has already progressed.
The status quo: Instead, doctors send patients with mild cases of COVID-19 home to isolate, advising them to call in if they start to feel worse. The doctor can then decide whether they should come in for a visit or be hospitalized based on their self-reported condition.
The problem with this is that a patient might not feel worse until after their illness has already progressed — symptoms often lag behind the virus’s progression. People also might wait to call a doctor, thinking worsening symptoms aren’t severe enough to report.
By the time a patient is hospitalized, treatments may not be as effective.
The Telecovid study: Now, Technical University of Munich (TUM) researchers have tested a different way for doctors to remotely monitor COVID-19 patients.
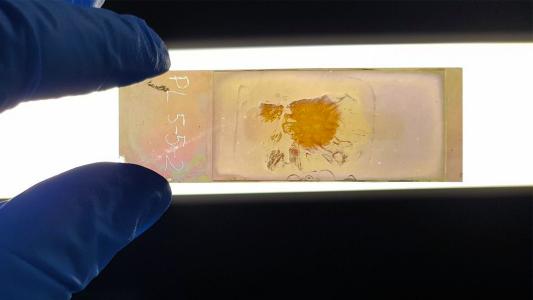
It’s a $150 ear sensor that’s worn like a hearing aid. The device collects patient data every 15 minutes and sends it to healthcare workers. Those workers can then look for signs that the patient’s condition is getting worse and hospitalize them, if necessary.
“To our knowledge, this is the first study worldwide to continuously monitor patients in home isolation remotely and to prompt immediate hospitalization in the event of critical health deterioration,” researcher Georg Schmidt said in a press release.
About 90% of the trial’s hospitalized patients said they would have delayed going to the hospital.
The results: TUM’s Telecovid study included more than 150 high-risk COVID-19 patients. Each wore the ear sensor for about 14 hours a day and was monitored for about 9 days.
The device measured a patient’s temperature, blood oxygen level, and more every 15 minutes and sent the data to healthcare workers. If they spotted signs that a patient was deteriorating, a doctor would call the patient to discuss hospitalization.
Twenty patients were hospitalized during the study, and decreasing blood oxygen levels were the primary indicator that their condition was getting worse. Seven of the hospitalized patients were ultimately admitted to the ICU, and of those, one person died.
The impact: The study lacked a control group, so it’s not clear if the ear sensor actually led to better patient outcomes.
However, about 90% of the hospitalized COVID-19 patients said they would have delayed going to the hospital if they hadn’t been a part of the Telecovid study, and the majority of those admitted to the ICU said they didn’t realize the severity of their conditions.
“After discharge from hospital, all patients declared that they were convinced that the hospitalization prompted by the Telecovid team had improved their chances of recovery,” the researchers wrote.
At the very least, such remote sensors may offer a way for overwhelmed healthcare systems to triage without overlooking patients in need of care.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].