Researchers around the world have been racing to develop new vaccines, antivirals, and other therapies to blunt SARS-CoV-2’s attack, even while the virus evolves to become an endemic problem.
While existing vaccines are capable of reducing severe cases of COVID-19, at least with a recent booster, continued mutations and the difficulty of maintaining high booster rates mean that better defenses will need to be developed.
“Vaccines are making a huge difference, but vaccines are not universal, and there is still a tremendous need for other approaches,” Anders Näär, a professor of metabolic biology at UC Berkeley, said.
While existing vaccines are capable of reducing severe cases of COVID-19, continued mutations and the difficulty of maintaining high booster rates mean that other defenses will need to be developed.
Näär and his Cal colleagues’ approach uses inhalable, DNA-like molecules to throw a wrench into the coronavirus’s replication machine.
“A nasal spray that is cheaply available everywhere and that could prevent someone from getting infected or prevent serious disease could be immensely helpful,” Näär said.
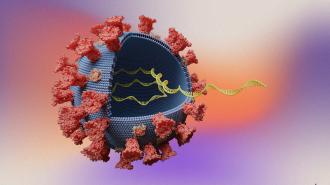
Gumming up the works: The Berkeley team’s nasal spray, published in Nature Communications, uses short snippets of synthetic DNA called “antisense oligonucleotides” — or ASOs for short.
ASOs can be programmed to glom onto specific strings of RNA — blocking them from being copied or turned into proteins.
Näär has been studying the use of ASOs for over a decade, trying to figure out how to use them to affect RNA involved in conditions like type 2 diabetes, Duchenne muscular dystrophy, and fatty liver disease.
But when the pandemic hit, they set their sights on a different type of RNA — virus RNA.
“The SARS-CoV-2 genome is single-stranded RNA, similar to messenger RNA or microRNA,” Näär said. “We thought perhaps we could use these ASOs to stick onto the viral RNA and prevent it from working.”
The nasal spray uses DNA-like molecules to gum up SARS-CoV-2’s replication.
The hairpin bend: Working with the Innovative Genomics Institute and Berkeley researcher Sarah Stanley’s lab, the team sicced hundreds of different ASOs — all designed to attack different parts of the genome — on SARS-CoV-2.
One target in particular proved effective: a non-coding portion of the virus’ RNA that forms a hairpin and seems to play a key role in replication. With an ASO stuck to its hairpin, the virus was unable to replicate.
The ASOs stopped the coronavirus from replicating in human cells in the lab, and in animal experiments, it both prevented infection, when given early, and treated COVID-19 after infection.
“We showed that if you bind an ASO to this hairpin, it dissolves the hairpin, and the RNA forms a straight line instead of a bubble structure,” Näär said. “We think that this prevents the virus from effectively translating and replicating, and we found that it was incredibly effective at preventing viral replication in human cells.”
When sprayed in the noses of mice and hamsters, the ASO protected against and treated COVID-19, but just as importantly, it did not spark an immune response of its own — suggesting it likely won’t cause toxic side effects in people.
The hairpin is found in all known variants of SARS-CoV-2, and the team’s ASOs were shown to be effective against variants of concern, including Delta and Omicron.
“A nasal spray that is cheaply available everywhere and that could prevent someone from getting infected or prevent serious disease could be immensely helpful.”
Anders Näär
Next steps: ASOs are stable and relatively cheap to produce at scale, the researchers said, making them a potential boon for fighting the virus around the world.
They’re also a promising way to attack other RNA viruses, like influenza, RSV, and other respiratory viruses, since they can be designed to stick to any RNA genome. The team has already found an ASO which sticks to a target in SARS-1, and they have begun preliminary work on influenza.
More research will be required before human clinical trials can begin, though.
“It’s very clear that this virus is not going away,” Näär said. “We need a lot of different avenues to tackle it, and therapeutics like ours that are agnostic to the variants could play a major role.”
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].