Most people with chronic back pain naturally think their pain is caused by injuries or other problems in the body such as arthritis or bulging disks. But our research team has found that thinking about the root cause of pain as a process that’s occurring in the brain can help promote recovery. That is a key finding of a study my colleagues and I recently published in JAMA Network Open, a monthly open-access medical journal.
We have been studying a psychological treatment called pain reprocessing therapy that may help “turn off” unhelpful and unnecessary pain signals in the brain. To do this, we carried out a study in which some people were randomly chosen to receive the pain reprocessing therapy treatment, while some got a placebo injection into their backs.
We included 151 adults ages 21 to 70 years old with chronic back pain. We found that 66% of participants reported being pain-free or nearly pain-free after pain reprocessing therapy, compared with 20% of people who received a placebo.
These results were remarkable because previous trials of psychological treatments rarely led to people reporting full recoveries from chronic pain. So we needed to better understand how this treatment worked: What changed in people’s thinking that helped them recover from chronic back pain?
Why it matters
Chronic pain is one of the biggest health problems today. It is the leading cause of disability in the U.S., and it has an economic cost greater than that of diabetes or cancer.
The most common chronic pain condition is back pain. Many patients – and doctors – are focused on identifying different back problems that they suspect may be causing the pain. So they try all sorts of treatments, often to no avail.
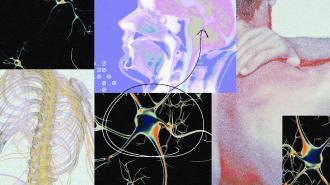
A growing number of scientists now believe that many cases of chronic back pain are caused primarily by brain changes. Pain can originate with an injury, but then the pain system can get “stuck” and keep firing long after injuries have healed.
Pain is the brain’s alarm system, letting us know about injuries or other threats to our body. Much of the time, the system works well, accurately warning us that a part of our body is injured and needs to be protected. But when a person has been in pain for months, years or even decades, pain processing pathways are more likely to fire, and brain regions that typically are not involved in pain start to be involved. Chronic pain also leads to increased levels of activity in glial cells, which are part of the brain’s immune system. All these changes in the brain then serve to “entrench” the pain, making it persist.
People, very understandably, think that if their back hurts, there must be a problem in the back – even though we researchers know this is often not the case.
It’s critical to note that just because the signal originates in the brain, the pain is not any less real. The pain is always real, no matter what. But to treat it effectively, one needs to accurately identify the root cause.
How we do our work
In our study, we asked people to tell us in their own words what they think is the cause of their chronic back pain. It is a simple question, but few studies have asked their participants to describe the source of their pain.
Participants in our study described injuries, weak muscles, arthritis and other bodily factors as the causes of their pain. Almost no one mentioned anything about the mind or brain.
One of the main goals of pain reprocessing therapy is to help people think differently about the causes of their pain. After we treated participants with pain reprocessing therapy, about half the causes of pain that people described were related to the mind or brain. They said things like “anxiety,” “fear” or “neural pathways” were the causes of their pain.
The more that people shifted to this kind of understanding, the more their back pain went down. We think this shift in understanding reduces fear and avoidance of pain, which can tamp down pain pathways in the brain and promote healthy, pain-reducing behaviors like exercise and socializing.
Ask your health providers, or check out these online resources that can help you assess whether and when the brain is playing a role in chronic pain.
Accurately identifying the underlying causes of pain is the first step toward healing it.
The Research Brief is a short take on interesting academic work.
This article is republished from The Conversation under a Creative Commons license. Read the original article.