Using stool and blood samples collected more than 35 years ago, researchers have found a connection between the collection of bacteria in a person’s gut and their chances of getting HIV — and this link could help in the fight against AIDS and other diseases.
The background: AIDS was still largely a mystery in the early 1980s — we didn’t know what caused it, how it was transmitted, or how to prevent it. But one of the few things scientists did know was that it disproportionately affected men who had sex with men.
“Let me tell you, there was some pressure to throw this stuff out.”
Charles Rinaldo
In an attempt to learn more about the cause of AIDS, the NIH funded the Multicenter AIDS Cohort Study (MACS) in 1983.
The study initially enrolled 5,000 gay and bisexual men, all of whom agreed to submit biological samples (blood, urine, stool, etc.) at collection sites in four cities every six months. None of the men had AIDS at the beginning, but some contracted it during the course of the study.
The samples: The University of Pittsburgh was one of the MACS collection sites, but even after HIV was identified as the cause of AIDS, their samples were not destroyed. Instead, they were cryogenically frozen and stored for future research.
“Let me tell you, there was some pressure to throw this stuff out,” Charles Rinaldo, a professor of infectious diseases at Pitt, told Axios. “It costs a lot of money to keep these for 35 years … I was one of the people that said ‘No way.'”
“MACS had, thankfully, preserved a treasure trove of specimens.”
Shyamal Peddada
The idea: In 2017, Rinaldo discussed the MACS samples with then-Pitt colleague Shyamal Peddada, who had expertise in the unique collection of microbes living in our gastrointestinal tracts, known as the gut microbiome.
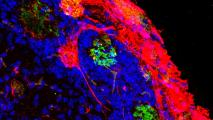
In recent years, scientists have started to realize that the gut microbiome can affect everything from brain structure to the success of cancer treatments, so the two got the idea to use the samples to see what impact, if any, it might have on a person’s chances of getting HIV.
“It became apparent to both of us that MACS had, thankfully, preserved a treasure trove of specimens,” Peddada said. “Science had advanced to the point that we could now revisit this biorepository to find out what was happening in the microbiome and immune system of men before and after they got HIV.”
HIV progressed to AIDS more quickly in men with “unfavorable” gut microbiomes.
The discovery: The team analyzed blood and stool samples from 265 participants who were HIV-negative at the start of the study. Of those, 109 contracted the virus before the end of the sample collection.
They discovered that men who contracted HIV had higher levels of a bacteria linked to inflammation in their gut microbiome and lower levels of four bacteria linked to immune response. They also had higher levels of inflammation in their blood prior to contracting HIV.
Among those who ultimately got HIV, those with these unfavorable microbiomes also saw their disease progress to AIDS more quickly than HIV-positive men with more “normal” guts.
“If the gut microbiome influences a person’s susceptibility to HIV in this way, it could be doing the same for other pathogens.”
Charles Rinaldo
The cold water: Anyone can contract HIV, but the researchers only had access to samples from gay and bisexual men. That means we don’t know for sure that the insights from their study translate to the population as a whole, particularly to women.
It’s not clear how we might be able to find out, either, since many high-risk people now take PrEP meds, which dramatically lower their chances of getting HIV. However, PrEP has been shown to affect the microbiome, which would complicate the results.
The big picture: The newly discovered link between the gut microbiome and HIV susceptibility reveals a new dimension of disease transmission and resistance, which could lead to new prophylactics and treatments. It might also help researchers combat other viruses.
“If the gut microbiome influences a person’s susceptibility to HIV in this way, it could be doing the same for other pathogens, such as COVID-19,” Rinaldo said.
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].