A handful of studies are investigating the use of electrical brain stimulation as a long COVID treatment, attempting to alleviate the neurological symptoms being reported by patients.
Although small in scale, pilot trials being performed by NYU and the Medical University of South Carolina have pointed to the potential therapy as being safe to do at home, and patients have reported signs of improvement.
The work is indicative of the struggle medical science has with the long-term impacts of disease — called “sequela” — in the wake of viral infections.
“We need to do so much work to understand what long COVID is,” NYU neurology professor Leigh E. Charvet told IEEE Spectrum’s Eliza Strickland. “But we also need to reach people now with something that we know is safe and deployable.”
Researchers are not sure what causes some patients to develop long COVID while others recover quickly and completely.
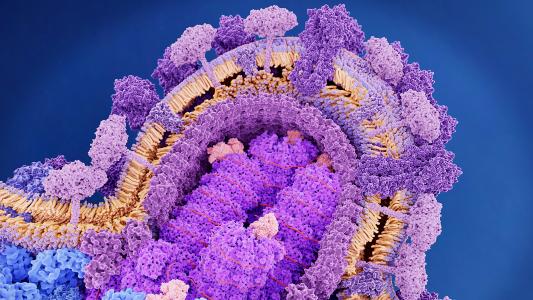
SARS-CoV-2’s lingering effects: It is not unprecedented for a viral infection to lead to health impacts that can drag out over months, or even years — some patients of the original SARS suffered chronic fatigue and reduced lung function even four years past their recovery.
Unfortunately, not only are these conditions not very well understood, but patients can also find themselves being dismissed by their doctors, their conditions dubbed psychosomatic out of hand.
But the sheer number of COVID-19 cases happening in a small, well-watched window has thrown sequela into sharp focus.
Now called Post-acute Sequelae of COVID-19 (PASC), researchers are still not sure what causes some patients to develop long COVID while others recover quickly and completely.
Potential PASC causes can include direct tissue damage from the infection, other pathogens taking advantage of the immune system being shaken up, and autoimmune issues developed in the wake of infection. And those are just a few of the theories.
So, we don’t have a definite or single cause. And to make long COVID treatment even more difficult, patients present many different symptoms, from persistent shortness of breath and fatigue to neurological issues, especially brain fog and difficulty regulating their emotions.
Creating a long COVID treatment for so many different symptoms is hard enough; to do so without a strong understanding of why long COVID is happening is even more difficult.
“It’s a very heterogenous group of people describing very heterogenous symptoms,” NYU neurology professor Jennifer Frontera told Spectrum’s Strickland. Researchers are trying to get to the bottom of the problem, with $1 billion pledged to the task.
But it’s the neurological symptoms which Frontera is most concerned about, she told Strickland.
“We don’t have a medication for brain fog.”
Patients present many different symptoms, making long COVID treatment even more difficult.
A shocking long COVID treatment: The NYU and South Carolina groups are testing two different types of brain stimulation as a potential long COVID treatment for those neurological symptoms.
The methods are different from deep brain stimulation (DBS), where implanted electrodes deep in the brain can treat Parkinson’s tremors and epilepsy, among other things.
Instead, Charvet’s group is using transcranial direct current stimulation (tDCS), where subjects wear what is essentially a headband that sends the current to the brain through the scalp. It’s a safe, noninvasive way to provide electrical stimulation (albeit much weaker than DBS).
Mark George, at the Medical University of South Carolina, is using a device that stimulates an important nerve called the vagus nerve, which plays a role in regulating internal organ function, via the ear.
Charvet began testing tDCS as a long COVID treatment after the first wave of patients began coming to her neurology clinic in the spring of 2020. “They were saying, ‘I can’t function, I can’t return to work,’” Charvet told Strickland.
The handful of patients Charvet has worked with so far use the tDCS from their house. They put the band on, call the research group, and are given a code which activates the specific stimulation for them. While they go through their 20 minute session, they also do some kind of activity, like a cognitive game, and may follow up with physical exercise, Strickland reported.
Charvet’s patients have seen their conditions improve, enough so to support doing larger studies to dial-in the treatment and test its efficacy.
Although small, the trials show that brain stimulation could be done safely at home, and the limited patients enrolled have reported an improvement in symptoms like brain fog and anxiety.
Early days: It’s important to note the current limitations of the work; it’s far too early to say tDCS is an effective long COVID treatment. Her current trials are more “a testing ground—it’s not scientific, it’s not controlled,” Charvet told Strickland.
Geroge’s patients reported improvements in brain fog, energy, and anxiety as well. The South Carolina group did hour-long sessions of vagus nerve stimulation while using wearable sensors to measure heart rate, blood pressure, and oxygen saturation. While larger trials are necessary to figure out if this method is actually working better than a placebo, the safety data is promising.
“We showed you could do this kind of stimulation at home; the safety data was impeccable,” George told Strickland.
Both George and Charvet are planning larger trials designed to test if electrical stimulation may actually be an effective long COVID treatment; as with many things in medicine — and COVID in particular — only time and more, better data can tell.
“What drives us is that there’s a tremendous unmet need,” Charvet said. “And our patients are getting better.”
We’d love to hear from you! If you have a comment about this article or if you have a tip for a future Freethink story, please email us at [email protected].